Two down, one to go. Knee replacement surgeries, that is.
After Jim and I both had to stop running several years ago, we used
to joke that we had only one good knee between us.
It was one of Jim's knees. He'd already wrecked his other one.
Several years ago he had a nasty bike accident and
damaged the meniscus in one knee. Surgery to repair the meniscus wasn't successful
enough to allow him to resume running. Before long, the cartilage wore
down enough in one compartment of the knee that it was painful for him to
walk. So last December he had a partial knee replacement to fix it.
Here's what it looks like in an x-ray:

Meanwhile, previous to that I had already learned back in
2009
that I was at or near being "bone-on-bone" in both
knees due to osteo-arthritis, the most common form of arthritis as we
age and our cartilage wears out.
I began
getting viscous gel injections every six to eight months in both of my
knees, a treatment called visco-supplementation. The brand I used most
often was Orthovisc, given once a week in both knees for three weeks by
my orthopedist in Roanoke, VA. While traveling around the continent in
our RV the last 13 years, other orthopedists occasionally gave me Synvisc, GelOne,
or Hyalgan if we weren't in Virginia when I needed more injections. There
are other brands of gel, too.
I was lucky those injections worked
very well to relieve all or most of my knee pain for about six years.
Then rather suddenly the gel reabsorbed faster than six months.
That's the minimum length of time between injections that insurance companies and Medicare
will pay for these expensive treatments.
For the last two years I got an interim cortisone (steroid) injection
between gel injections to keep the pain at bay.
Then rather suddenly this summer that didn't work either. The
cortisone didn't last more than a few weeks and it wasn't safe to get
more until three months had elapsed. My knees hurt so badly I couldn't
walk for exercise, even if I took a Tramadol pill (a rather mild opioid
pain reliever), let alone with the generic ibuprofen or acetaminophen
I'd been using for many years.
That's when I knew all of my non-operative treatment options had run
out and I'd need two total knee replacements.
Fortunately, I knew who to call!
[Warning: This entry is long on verbiage -- that I hope
will be helpful for other folks who are considering knee replacements -- and shorter
on relevant photos and graphics. I will divide the introduction, surgery, and
recovery into four pages so they are faster to download and easier to read.]
STEP ONE: FINDING A SKILLED SURGEON
This could have been very time-consuming since we've recently moved
to a new area. I totally lucked out without even trying -- and
before I even knew I needed a knee replacement surgeon yet!
One of the first neighbors we met when we moved to Peachtree City at
the end of March is a retired couple living in the house three doors
down the street from us. They were walking by our house one morning and
saw the Leadville 100 shirt I was wearing. Their son, who was visiting
from N. Georgia, recognized this popular endurance cycling and running race; he's a runner.
When I mentioned that I don't run any more and would probably need
knee replacements in another year or two, Gail quickly said she had a wonderful
orthopedic surgeon who did one of her knees three years ago, Dr. Todd
Schmidt with Ortho Atlanta.

She highly recommended him for his extra-minimally-invasive surgery
technique that allowed her to recover faster than the average patient.
Dr. Schmidt is reportedly one of only 15% of orthopedic knee surgeons
who use a more time-consuming and difficult procedure to spare as many
nerves, muscles, tendons, and ligaments as possible.
Gail is physically active, which also helped her recover more quickly.
I made an appointment to see Dr. Schmidt in early June to get interim
cortisone injections in both knees; my insurance wouldn't pay for
more Orthovisc or Synvisc gel
until September. At that point I assumed the cortisone would last until
September -- it had lasted three months previously.
I knew the hand-writing was on the wall, however, so I asked him
-- as I've asked other orthopedists I've visited in recent years while
traveling around the country -- how I'd know when it was time for a total
knee replacement. I already knew I was bone-on-bone in two compartments
in both knees so I wasn't a candidate for a partial knee replacement like Jim had.
I also knew I wanted to be in good physical shape when I had surgery,
which meant doing it before my knees hurt so badly that I couldn't walk or
cycle enough to be fit. A fit patient always does better during and
after surgery than an unfit one.
Dr. Schmidt basically said I'd know when I needed knee surgery!
He explained that when my quality of life was compromised, when I
could no longer walk, cycle, and participate in other activities like I wanted, it was time for surgery.
In no way did he push for surgery, even though he's done thousands of
total knee replacements during his career and plans to do a bunch more. He encouraged me
to wait until more conservative treatments like the gels and cortisone no longer worked but said the
damage to my knees was already advanced enough to justify surgery if I
decided to have it done.
My knees soon felt better with the cortisone and I was able to
comfortably walk, cycle, do gardening chores, etc.
I knew I'd probably need knee replacements in the next year or two, though.
BELIEVE ME, YOU'LL KNOW
I was pretty surprised when both knees began hurting five or six
weeks after that. Gels and cortisone were no longer the answer, nor the
other conservative treatments I'd used before that like physical therapy,
reducing the miles I ran and cycled, and taking OTC pain meds.
Rather suddenly I knew it was time!
I called the doctor's surgery scheduler, got a date for surgery about
six weeks later, and prepared myself mentally and otherwise for the
first of two total knee replacements.
It really helped me to have a positive attitude about surgery because
I'd been involved in the whole process last winter with Jim.
There were some differences, of course, because he had a partial and
not total knee replacement but they are similar invasive procedures.
In addition, we were spending the winter in SE Georgia then. His
doctor and hospital were in Brunswick, his physical therapist in St. Marys.
I'd be having my surgery in metro Atlanta with a different doctor and hospital.

Part of the Piedmont Fayette Hospital
complex where I had my surgery
Each doctor, hospital, and PT does things a little differently but
there were enough similarities that I almost felt like I'd been there,
done that. That experience as a wife and recovery "coach" were valuable
when I became the patient.
Another reason I was ready to make the decision to have surgery is
that just about everyone I've ever talked to who
has had one or two knee replacements has said they only wish they'd had surgery
sooner because they were able to resume doing the things they wanted
to do -- after full recovery -- without pain.
I haven't known anyone in recent years who regretted having the
surgery and very few people said they had such a bad experience
that they decided against having their second knee done, if it needed fixing.
I also heard more kudos as I was awaiting surgery from new friends
and medical providers in this area re:
Dr. Schmidt's expertise. Having faith in your doctor is very helpful
through the whole process.
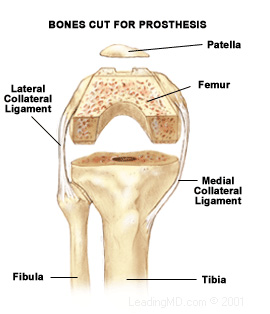
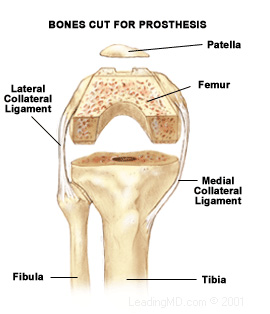
WHAT EXACTLY IS A TOTAL KNEE REPLACEMENT?
This is the lay term for the surgery that involves replacing a
seriously arthritic or otherwise damaged knee with an artificial joint made of
metal and plastic.
The correct medical term is "total knee arthroscopy," or TKA.
The surgeon removes diseased and damaged cartilage and bone in the knee
and replaces it with a prosthesis, or implant. The lower part of the implant is inserted (rather
forcefully!) into the tibia. The upper part is cemented to the femur.
Some folks need a third small implant behind the patella if it is badly
damaged. Remaining bone eventually grows around the pieces of the
implant and helps hold them in place.
Here are two images from the Ortho Atlanta
website that show the process:
You can find a lot of good information about total knee replacements on
the internet with a simple search of the topic. Choose websites that are
the most likely to be reputable, like the American Academy of
Orthopaedic Surgeons or the Mayo Clinic.
You can also find hundreds of videos on the internet that show all the gory details of
both partial and total knee replacement surgeries. Jim watched several of them
before his surgery last winter.
I
still -- five weeks after my first knee replacement --
have not watched any of those videos nor do I intend to do so before my second knee
replacement. It's graphic enough to see pictures like these and my own
X-rays. I don't need to see the medical team cutting my knee open or hear them hammering the tibial component
into my bone!
ALMOST DE RIGEUER?
Knee replacement surgeries have become rather commonplace in this
country as techniques and replacement materials have improved in recent
years, more surgeons have more practice, and more Gen Xers, Baby Boomers, and
members of The Greatest Generation have worn out their knees due to
aging, lifestyle (including athletic injuries and overuse), and the obesity epidemic.
Over 700,000 knee replacements were performed in this country in 2016.
It's almost become "fashionable" to say you've had one!
The surgery has a high success rate. Every surgery has risks but the
risks of infection, blood clots, or something else going wrong during and after total
or partial knee surgery are low if patients and medical personnel follow
all the recommended procedures.
Dr. Schmidt is very concerned about positive outcomes so he has some
strict pre- and post-operative "rules" for his patients to follow.
The hardest one I've had to overcome is his requirement that I wait at
least three months before having my second knee done, even though my
recovery from the first surgery has been faster than average for a
68½-year-old woman. I'd have it done tomorrow if he'd do it.
I have to realize that the doctor has my best interest at heart. Despite
the fact that I was able to meet my physical therapy goals in only five weeks
and have been released on my own recognizance, there are things inside my
aging body that I can't see that must thoroughly heal before it's wise to
go through the whole process again with my other knee. <big sigh>
One reason I'm glad I was able to wait as long as I have for knee
replacements is the average life span of the prosthesis --
anywhere from 10 to 20 years, depending on level of activity and other
factors.
Reportedly 90-95% of knee replacements last 15 years. The older a person
gets, the harder surgery is, so I hope my new knees last even longer
than that. With all the medical and scientific advancements in knee
replacements I'm surprised implants don't last longer by now.
Activities that involve pounding, like running, only shorten the
lifespan of a knee replacement. As important as ultra-distance running
was to me for 30 years, I will never run again. I won't even walk
ultra-marathon distances again, either.
And that's OK. I've already proven to myself that I can run and walk
distances most people don't even like to drive.
I'd rather walk, hike, cycle, and kayak more conservatively
from now on and still be mobile in my 90s.
PRE-OP MEDICAL APPOINTMENTS
I didn't see Dr. Schmidt again after my initial appointment for
cortisone and advice until the morning of surgery, three-and-a-half months later.
That was OK because he has an excellent medical team with a nurse,
two PAs, a surgery scheduler who arranged several other appointments for
me, and a "care coordinator." They were able to answer all my questions
and gave me lots of information.
The hospital (Piedmont Fayette) also has a team approach with surgery
staff, nurses, nurse assistants, physical therapists, and the department
coordinator who teaches the required "joint class" for hip and knee
patients.

A little orthopedic humor at the
hospital
Within 30 days of surgery I had several pre-op appointments:
1. Surgery clearance by a Primary Care Physician of my choosing. Jim
and I needed a PCP in this area anyway so this prompted us to do our
research PDQ. We chose a female doctor in town that we both really like because
she's so thorough and responsive. My EKG, blood work, etc. came out fine
and I was cleared for surgery without having to see a cardiologist.
(Jim had to see one before his surgery but he was cleared for it after
further testing.)
2. Pre-op appointment with one of Dr. Schmidt's PAs. X-rays were
taken of both knees/legs. The PA asked a lot of medical questions,
answered my questions (I had a long list), and gave me more
information about what I needed to do prior to surgery, like what meds
and supplements to stop taking and when. I signed consent forms and
got scripts for post-surgery pain meds.
3. "Joint class" at the hospital three days before surgery. This was
similar to the class I attended at the hospital in Brunswick with Jim.
It's a pre-operative education class so patients and their "coaches"
(the person who will be with them after surgery) know what to expect
before, during, and after surgery. I was required to go to Jim's class but
he didn't have to go to class with me here. That's fine, because I could
tell him what differences there would be between the two hospitals' procedures.
4. Pre-admission testing at the hospital right after the joint class,
which was a thorough review of my medical history and current vitals
(blood pressure, temperature, oxygen level, pulse).
Another one of my neighbors was the nurse supervisor for the
orthopedic wing at Piedmont Fayette Hospital for many years. She's retired now but told
me to mention her name to the staff while I was there. The pre-admission
nurse, joint class nurse, and nurses who took care of me overnight in
the hospital after surgery all know and like her.
Having that connection, and knowing this is a nationally top-ranked
hospital, also helped alleviate most of my concerns about having surgery.
From the surgeon to the hospital staff, I assumed I was going to be in good hands.
PREPARING FOR SURGERY & RECOVERY @ HOME
We got plenty of information well before surgery about how to prepare
ourselves and our house for the recovery phase.
Since I have a spouse to take care of me after surgery and don't live
alone, I knew I'd be recovering at home after surgery and wouldn't have
to go to a rehabilitation facility or have professional in-home nursing
care the first two or three weeks.
We also knew most of
Dr. Schmidt's patients go home the day after surgery. That's one of
the nice things about his extra-minimally-invasive technique
-- usually only one night required in the hospital.
Prior to surgery I had a lengthy phone conversation with my "care
coordinator" at Ortho Atlanta to be sure everything was in place when I
got home. Some of her questions specifically dealt with mobility issues
after surgery -- do I already have a walker and cane? do we have
steps? are there throw rugs that might trip me up? how easy is it to get
into and out of our car? do we have any pets?
Ha! Pets.
That was the only real obstacle I presented. I told her about all of our
"dogs on the floor" (see last journal entry about our three Labrador
retrievers) but assured her Jim and I had already discussed that issue pretty
thoroughly so I would be at low risk of falling.

Can I help it if I'm the
Pied Piper? They like to follow me wherever I go.
Since Jim would need to be at the hospital most of the day of
surgery, we arranged doggie day care and possibly overnight boarding for
Casey (5-year-old Lab) and Holly (just 16 weeks old,
but had completed all her shots that week). We had time to get them to
day care before I checked in at the hospital and Jim was able to
retrieve them later in the afternoon so they didn't have to stay
overnight. They went back to day care the next day when Jim came back to
the hospital for three hours.
I didn't know if I'd be able to
stand up very long to prepare meals the first few days at home so we
went on a cooking frenzy prior to surgery. We made six of our favorite
dinners with four servings (or more) in each = a lot of meals. We froze
them to make it easier on both of us the first couple of weeks.
Turned out, we made more than we needed. I would have been
able to prepare meals just fine the second week but it was nice having them already made.
I have several loose-fitting athletic and lounge pants so I didn't
need to purchase any more clothes to fit over my swollen, bandaged knee.
The weather was warm enough to wear shorts anyway.
I didn't need any new shoes, either. Most of the time since surgery I've been
wearing two different pairs of Keen athletic sandals rather than running shoes. The
sandals are easy to get on, accommodate a swollen foot, and
are comfortable enough to walk or cycle on the paved bike paths in our neighborhood.
Continued on the next page: day of surgery and the next day
Happy trails,
Sue
"Runtrails & Company" - Sue Norwood, Jim O'Neil,
Cody, Casey, and Holly-pup
Previous
Next
© 2017 Sue Norwood and Jim O'Neil