Let me preface this by saying I'm not a doctor . . . and I don't play one on TV!
This entry is all about the impinged ulnar nerve in Jim's right arm.
It didn't exactly "tickle his funny bone," but instead has caused
significant muscle deterioration and weakness between the thumb and
forefinger in his dominant hand, plus numbness and tingling in his outer
fingers when cycling.
After a nerve conduction test and physical examination by an
orthopedist who specializes in hand surgery, his condition was diagnosed
as Cubital Tunnel Syndrome AKA Ulnar Nerve Entrapment.
Graphic from the link in the quote at the top of the page
His hand got so bad that non-surgical treatments weren't effective,
so Jim decided to have surgery to release the nerve in both his elbow
and his wrist several weeks ago.
The good news is that his recovery is going well. Only time and
consistent home physical therapy will tell if the muscles are able to
rebuild their mass and strength between his thumb and forefinger. The
numbness/tingling in his fourth and little finger is gone.
This is not a well-known medical condition, so I'll try to describe
it here from our lay persons' perspectives and the help of the internet.
CARPAL VS. CUBITAL
Most folks have heard of carpal tunnel syndrome, which is
often caused by too many repetitive motions like using keyboards on computers and
other electronic devices. There are other causes, too, as described on
the American Academy of Orthopaedic Surgeons' (AAOS)
website.
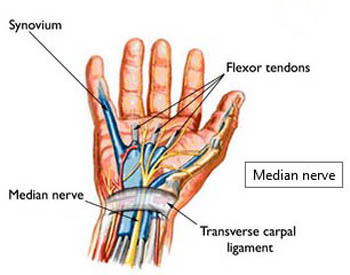
Pressure on the median nerve on the inside of the lower arm causes
swelling in the carpal tunnel, which results in pain, numbness,
tingling, weakness, and/or muscle wasting in the affected hand.
Here's a diagram from the AAOS link above of the median nerve
and carpal tunnel:
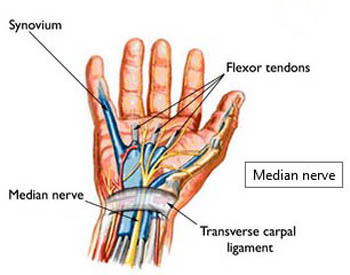
Treatment of carpal tunnel syndrome starts with conservative
non-surgical methods like braces, changes in activity, physical therapy, NSAIDs, and steroid injections.
If those aren't successful, surgery may be indicated to prevent
irreversible damage to the hand. The goal is to release the pressure on
the median nerve so it can function normally again after some time and physical therapy.
Most of the above is true for cubital tunnel syndrome, too,
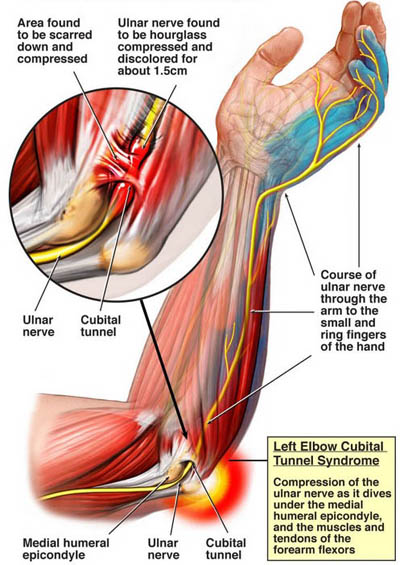
except it involves a different nerve, the ulnar nerve:
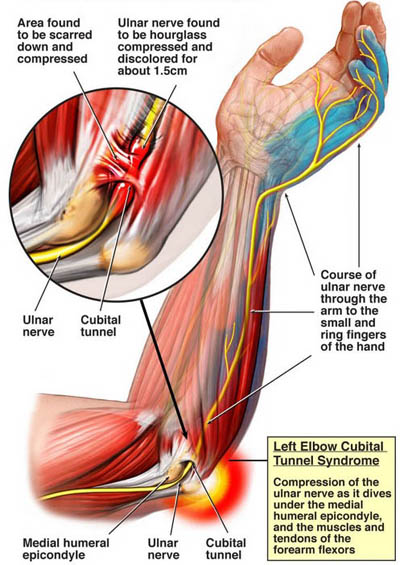
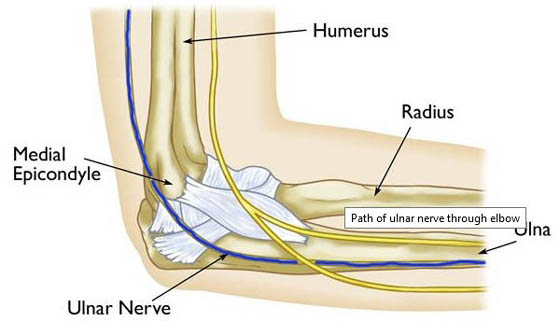
As you can see from the diagram above that I found during a Google search, the
ulnar nerve passes through the inside of the elbow at the cubital
tunnel, down the lower arm and through the another tunnel in the wrist
called Guyon's Canal, then leads
to the four fingers and the muscles between the forefinger and thumb.
Compression or stretching of this "funny bone nerve" can cause
numbness or tingling in the ring and small fingers, weakness/muscle
wasting in the hand, and/or pain in the forearm.
Jim had those first two symptoms, most noticeably in his right
(dominant) hand.
LOSING HIS GRIP?
Jim wasn't fully aware of the muscle wasting until our primary care
physician in Virginia pointed it out to him in a routine physical exam
about four years ago.
Jim mostly thought losing his strength and grip was part of the aging
process. At the time our doc mentioned the problem, we were focused on selling
our house so we could become full-time RVers. With that accomplished, we
began traveling all over North America for the next three years.

Worthington Glacier north of
Valdez, Alaska is in the background; that's our Cameo 5th-wheel.
(6-17-15)
Medical continuity was a challenge during that period of time, and
stopping long enough somewhere for surgery wasn't part of the our plan
unless absolutely necessary.
Jim's hand finally got so bad, however, that he decided to seek advice from
an orthopedist near our new home in October of this year. He consulted with
Dr. Virginia Jones, a hand specialist with the large Ortho Atlanta orthopedic
practice that has offices all over the metro Atlanta area.
(We've now seen four different orthopedists in this practice, for
various body parts and a nerve conduction test, and highly recommend them.)

Dr. Jones' initial exam included medical history and testing Jim's strength
and grip with both of his hands. His dominant right hand was much weaker than the
left hand and the muscle wasting (atrophy) in his right hand was also obvious
just by looking at the two hands.
Jim failed a simple grip test on the affected hand with
a piece of paper between his thumb and forefinger -- he couldn't firmly
grasp it like he could with his non-dominant hand.
My brother later quipped that he bet Jim would have held on tight if
a $20 bill had been used!

Yep, Jim might have latched onto one of
these
better than a blank piece of paper!
That day Jim got cortisone injections in both hands and a splint for
his left "trigger finger" thumb.
Cortisone has worked fairly well for both of his hands previously but it is
only a temporary solution for pain and doesn't address the deteriorating muscles
in his right hand at all. The splint has helped make the left trigger thumb more
comfortable as Jim waits to decide whether to have surgery for that problem someday.
NERVE CONDUCTION TEST
Dr. Jones described Jim's problem on his right hand as "peripheral neuropathy" but
she didn't diagnose Cubital Tunnel Syndrome for certain until he had a nerve conduction test a
few days later. She referred him to another orthopedic specialist in the Ortho Atlanta practice,
Dr. McHenry, for that test to give her more specifics about the problem with Jim's right hand.
Jim was apprehensive about having the nerve conduction test done but knew it was
necessary to pinpoint the problem and address it properly. He had terrible pain in
his neck and back a couple years ago after a nerve conduction test in Jacksonville and
swore he'd never undergo such testing again.
Fortunately, this time all went well -- he had no pain afterwards and Dr. Jones
got the information she needed to properly diagnose his problem and how to fix it.
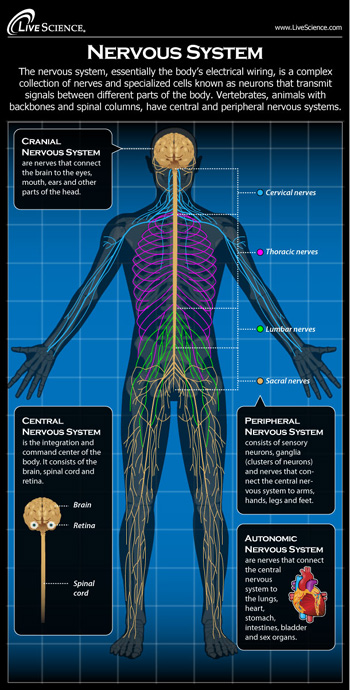
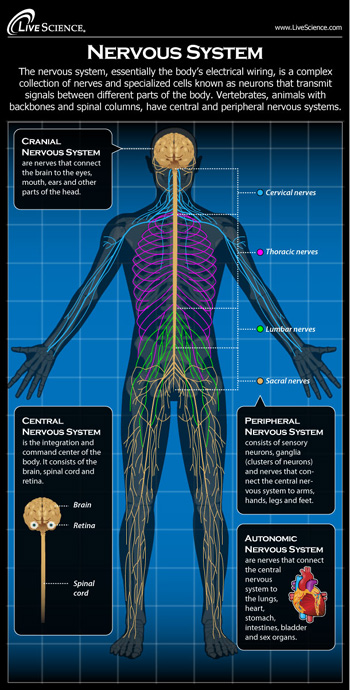
We truly are a bundle of
nerves!
This diagram is from the
LiveScience website.
Dr. McHenry explained after the nerve conduction tests that Jim had ulnar
nerve impingements in both his right elbow and wrist, not just the
cubital tunnel in the elbow.
When we went back to see Dr. Jones' PA a few days later, we learned that
Jim's best option would be surgery. Anything less than decompressing the
nerve in both locations would mean he'd continue to lose muscle mass and
strength in that hand. Further delay was not a good option.
Jim pretty much
decided then and there to schedule out-patient surgery with Dr. Jones at
the nearby hospital complex where I had my knee surgery.
I certainly
encouraged him to get it fixed once and for all. By that time I was
mostly back in commission around the house after having my first total
knee replacement so I could do more of the chores, drive short
distances, assist Jim with eating and dressing, etc. while he was
recovering.
This was his
dominant hand and arm, after all, so he'd be more limited in what he
could do for himself than if it was his other hand/arm.
IT'S A SMALL WORLD!
Jim's out-patient
surgery was scheduled for Friday, November 3.
In the intervening
time, he got medical clearance for surgery from our new primary care physician
and had his pre-op appointment with Dr. Jones. I went with him to
the appointment with Dr. Jones so I could learn more about the
surgery that would be done the next day.
Jim wore one of his Leadville
Trail 100-mile shirts to that appointment -- and Dr. Jones
noticed it immediately when she entered the room.
Would you believe,
her husband did the LT100 bike race in 2014!! Jim did it in 2013.

Jim powers
up to 12,600 feet elevation at Columbine
Mine during the
LT100 bike race on August 12, 2013.
We talked with Dr. Jones about the hundred-mile foot and bike races in Leadville for
a little while.
Small world. Who-da thunk?
Jim was relieved after talking with Dr. Jones more about the surgery even
though she didn't think she'd be able to use the least invasive of three
possible techniques to relieve the pressure on the ulnar nerve in the
elbow.
She wouldn't know exactly which technique was required until she
saw during surgery what was going on inside his elbow. The day before
surgery she thought he might be one of the 10% of patients with
similar symptoms and nerve-conduction test results that require the more
invasive surgery where the nerve has to be moved over about an inch.
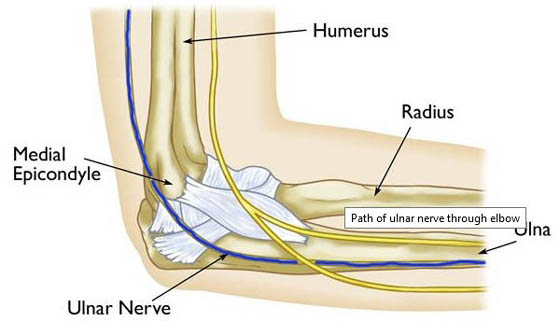
Normally the ulnar nerve lies in a groove on the inner side of the elbow. Here's
another graphic from the AAOS
website:
From what Dr. Jones said, even the technique that is most invasive and
slowest to heal sounds like it has an easier recovery period than what Jim had been
reading about and watching on the internet.
That says something about how much credence we should put in what we see on You
Tube! Sometimes it's very helpful but other times it just makes
us worry too much.
At that point we were hoping that Jim will have
more use of his dominant hand sooner than he thought he would. Even so,
we finished up some things around the house and yard the day before surgery that would
be impossible or difficult for Jim to do for several days or weeks after
surgery, like heavy lifting, vehicle maintenance, and yard work.
DAY OF SURGERY
Jim had to be at the out-patient surgery center at Piedmont Fayette
Hospital (next photo) at 8 AM. We took Casey and Holly, our younger Labrador
retrievers, to Puppy Tubs for day care first, then went to the hospital.

After check-in Jim had to wait about 50 minutes to go back for pre-op. The
chairs were comfortable in the waiting room and I had HGTV to watch, so the time went by
faster for me than for Jim.
No matter how "easy" any surgery may sound, there is always some
understandable apprehension. Jim just wanted to get it over with.
They called me back to see Jim after he was in his gown and an IV was
inserted in his hand but before he got a nerve block and good drugs to relax him. One of
the anesthesia team members came in to ask questions and get signatures
re: insurance, then Dr. Jones came in to talk with us.

Jim looks pretty relaxed and ready to go into
surgery. He never lost his sense of humor.
At this in-patient hospital and out-patient
surgery center all
the medical folks ask the patients for their name and DOB,
what it is that they're having done, and where on their body. They did the same thing in
September when I had my knee surgery.
It's
obviously to ensure they have the right patient, the right procedure, and the right
body part!
When Dr. Jones came in she asked Jim what he was having done and he
joked, "I thought you knew!" She laughed.
We like Dr. Jones. She's personable and just cool, and we feel more of a connection after
finding out her husband is an ultra-distance cyclist (he also runs). She
also knows her stuff. In eight years of doing hand surgery, she's performed
about 200 cubital tunnel syndrome procedures per year,
about 300 carpal tunnel procedures each year, plus other types of hand surgery.
The nurse asked me to go back out to the waiting room when Jim got his nerve block; he
went into surgery soon after that. After about 40 minutes I was called back to speak with the doctor.
She said everything went well during surgery and she didn't have to do
the most invasive procedure that would involve moving the nerve near the
elbow an inch over. She said the nerve was very "congested" at both the elbow
and wrist but she was able to release it in both places. She described it as the nerve saying,
"Ahhhh, I have room now!"

Incision for cubital tunnel release in Jim's elbow

Incision for the other tunnel release in Jim's wrist
Dr. Jones also
talked with me about wound care and what activities Jim could do until
he went back for his first post-op appointment. Then she returned to the operating room.
Jim was her sixth of eight surgeries that day.
After a few more minutes I was allowed to be with Jim in recovery. The nurse
took out his IV and he was able to get dressed. He was released
after a relatively short time in the recovery room. (Although he was
asleep during surgery, it didn't take very long so the anesthesia wore
off pretty fast.) We got a prescription for Tramadol for pain, and written
post-op instructions.
We left the hospital at 11AM, just three hours after our arrival, and went to
Subway to get enough of his favorite turkey sandwiches for lunch the next four days for Jim. We went to Puppy Tubs for
"the girls" (Holly and Casey) and got home before noon.
Not a bad morning, considering!
RECOVERY
Jim's recovery from this surgery was more inconvenient than painful.
For the next few days he iced his arm every waking hour as instructed and mostly sat on the couch
with his feet propped up, reading, watching TV, or dozing:

Holly-pup was especially curious about Jim's sling and the pillows
he used to elevate his arm as instructed to reduce swelling.
Jim's arm was numb from the nerve block until bedtime the first
night. He needed Tramadol for only a day or two, and just Celebrex and/or
acetaminophen to relieve the pain from the surgery (and various
arthritic joints) after that.
He wore the sling on his arm in bed for a few nights so he
didn't roll over and tear the incisions accidentally in his sleep.
He wore the sling less and less during the day as he was able to do more things
and didn't have to keep his arm stationary.
Until his first
post-op appointment, Jim was instructed to
move his arm and fingers as much as was comfortable to increase the blood flow
and range of motion but not lift anything that weighed more than eight
pounds. That's the equivalent of a gallon of milk.
With increased movement
of his arm, he had trouble keeping the ACE bandage on. After several
days of struggling with it, he kept it off some during the day and used it mostly
at night and in the shower to cover the gauze bandages on the incisions.

Although we used a large plastic
bag to cover the Ace wrap and gauze bandages when he took showers, he
sometimes got the incisions wet. We had to change the elbow and wrist
bandages at least once a day to keep the incisions clean. I don't know why
something like AquaCel bandages was not used; the AquaCel that
covered my long knee incision in September allowed me to shower with
ease and stayed intact for five days until I was supposed to take it off.
When Jim went back in for his first post-op visit, his
incisions looked good and nothing was mentioned about getting them wet.
No harm, no foul, just a PIA for us with the bandages.
OH, TO BE AMBIDEXTROUS!
Some activities were difficult or impossible for
several days after surgery because Jim's dominant hand was sore and even weaker than
before surgery. He also had to be careful not to tear the stitches out.
If you're like most people, you have a dominant
hand (and leg). If you're one of those people, just imagine what life
would be like if you had no or very limited use of that hand for a while.
How would you cut a piece of meat on your plate
into bite-sized pieces? How would you tie your shoes? How would you
unscrew a tight lid off a jar -- or your bottle of pain medicine?
Those pill containers can be hard enough to get into with two good hands.
Occupational therapy addresses these and other
issues if a patient will be handicapped in this manner for a longer
period of time or has no one at home to help him/her.
Fortunately, Jim didn't need that because his
limitations would be temporary and I was there to assist him. He was
also pro-active and initiated his own version of occupational therapy.

Right-handed people have a dominant left brain;
ambidextrous brains are more symmetrical.
For a couple weeks before surgery Jim was wise to practice
doing more things with only his left hand -- using a fork or
spoon to eat, brushing his teeth, combing his hair, typing on the computer and phone
keyboards, getting dressed and undressed, even going to the bathroom.
Yes, he was able to laugh about most of this,
although I'm sure he got frustrated sometimes at things that were
awkward or even impossible with just one hand. He knew it was just a
temporary condition.
I did what I could to
make things easier for him after surgery, like cutting his food into bite-sized pieces.
There was no way initially that he could cut a chicken breast, for
example. I unscrewed jar lids and
the tops of pill containers until he could grasp them with both
hands again. He also needed some assistance with tying his shoes for a few days,
putting bandages on, and covering his arm with a plastic bag for the shower.
Some things he simply could not
do for one or two weeks -- drive, lift more than eight pounds,
mow and do other yard work, ride his bike outside (he used the indoor
trainer as soon as it was comfortable), work on the vehicles,
climb the ladder into the attic, and some other activities.
All these restrictions were lifted after his post-op appointment with
Dr. Jones eleven days after surgery. She was pleased with his recovery
and rate of healing. His stitches were removed and Steri-Strips put over
the incisions; they stayed on a few days, then fell off as intended.
PHYSICAL THERAPY
A few days after his post-op visit with the surgeon, Jim had an
appointment with a physical therapist with Ortho Atlanta who also
specializes in hands. The goal is to build back the muscles that have
atrophied between the thumb and forefinger in his dominant hand.

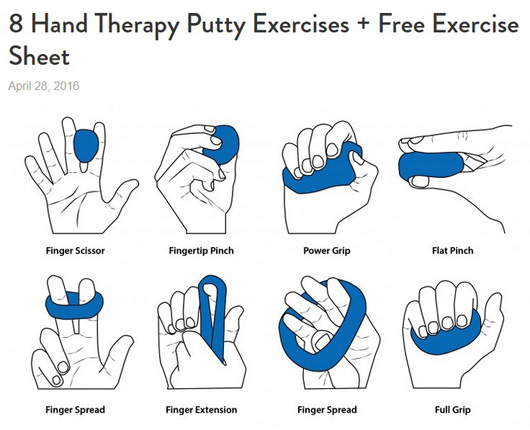
This putty is for PT, not for play.
That's the only formal session the therapist says he'll need as long as he
continues doing the strengthening exercises regularly -- and
maybe forever -- at home.
Instead of weights, balls, or stretchy bands, common physical therapy tools, he only
needs one glob of "hand therapy putty" material for his exercises.
It reminds me of the "Silly Putty" I used to play with as a kid.
Online you can purchase several different
colors from Amazon, Walmart, and other sources. Like therapy bands, each
color represents a different level of resistance. Jim's therapist gave
him yellow putty.
I found his sheet of
exercises online on the
FlintRehab site. It's the same sheet
Jim got from his therapist:
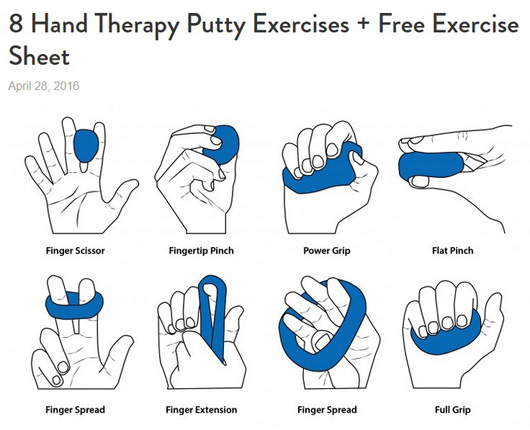
I assumed he'd have to use some sort of ball for his exercises. However,
squeezing a ball doesn't work to strengthen these particular muscles.
Apparently only hand therapy putty will do.
PROGNOSIS AFTER CUBITAL
TUNNEL SURGERY
According to Dr. Jones and what we've read on the internet from
reputable orthopedic sources, the results of each of the types of
cubital tunnel surgery are generally good.
As with any surgery, recovery from cubital tunnel surgery varies quite
a bit from one individual to another in regards to
which symptoms go away (numbness, tingling, muscle atrophy), to what
extent (from not at all, to totally), and how long it takes (from pretty
quickly to a long time -- or never).
The more fit you are, the better you'll recover
from any surgery.
We've had this book since 2008 and re-read it every
couple of years.
Our knee orthopedist recommends it to his patients,
too.
Cubital tunnel symptoms may not go away totally after surgery,
especially if the symptoms were severe. If the nerve was very badly
compressed or there was serious muscle wasting like Jim has, the nerve
may not be able to return to normal and some symptoms may remain.
Because nerves recover slowly, it may be a while before we know how well
Jim's ulnar nerve responds to surgery.
Since Jim has the beginning of the same symptoms in his other hand, he
is scheduled to have a nerve conduction test on his left arm and hand in
early December. He wants to get ahead of the damage in this arm/hand so
the muscles don't atrophy as badly as the one he had repaired.
Depending on the results of the test, he may have surgery on that
arm/hand in January or February. He won't know until he consults with Dr. Jones
again in mid-December.
It's been just three weeks since Jim's surgery. He has regained most of
the functional use of his right (dominant) hand and
has resumed all of his normal activities. The numbness and tingling in
his fourth finger and little finger disappeared soon after surgery;
that was a problem primarily when he was cycling.

Casey sure was happy when Jim could get back out on
his bike!
It will take a while to see
improvement in the atrophied muscles between his thumb and
forefinger. A lot will depend on how regularly he does his hand putty
therapy.
Next entry: We
got snow!! Photos from a rare, and fleeting, winter wonderland in Peachtree City
Happy trails,
Sue
"Runtrails & Company" - Sue Norwood, Jim O'Neil,
Cody, Casey, and Holly-pup
Previous
Next
© 2017 Sue Norwood and Jim O'Neil