As many problems as Jim and I have had with body mechanics and running injuries over the last three decades, you might wonder why we get so
much enjoyment from the sport of running (walking, hiking) very long distances! It
make us wonder sometimes, too, but we love it so much despite
the extra challenges that the main focus when we're injured is to rehab as
quickly as possible and resume running.
We are persistent!

Runner down, but only out a few weeks (October, 2004)
There are a lot of reasons why I'm not made for trail
running.
- I'm not the most coordinated person; it would be more sensible for me to stick to
smooth roads and greenways but they are often boring in comparison with trails.
- I'm genetically disposed to get osteoarthritis -- sure enough, I did
get it and now my knees prevent me from running like I want to.
- I get injured easily, usually from either clumsiness or over-training. In
retrospect, I would make a wild guess that I've been unable to run as much as
20% of the time the last thirty years because of injuries ranging from common
sore muscles and ankle sprains to more serious stuff like stress fractures (road
running days, not ultras), two torn tendons in one ankle (OK, that was an
ultra), and a toe that lost its mooring and had to be surgically re-anchored:

Toe realignment (October, 2004)
Name a running injury and I very likely have had it. In most cases, my
clumsiness or over-training has led to injuries. In some cases, the reverse has
been true -- my poor body
mechanics have led to injuries and/or surgery. In the case of the ruptured
ankle tendons, over-training → weakening
→ increased vulnerability and bad injury
when I fell into a hole on the
course → surgery
→ poor body mechanics ever since.
Although some of these things have led to rather vicious cycles, my goal is
always to get back out there and run again!
Jim's got the same mindset. He's definitely sturdier
and more coordinated than me but during his thirty-two years of distance running
he has had his share of injuries and mechanical problems, too. I think more of
his injuries have been caused by faulty mechanics than vice versa. He rarely
falls or strains an ankle; he's quite coordinated running on rough trails.

Who needs these stinkin' crutches?? I've got some races to
run!
(Jim after surgery
on both feet and calves in 2003; we still lived in Billings then.)
However, Jim has been
plagued with foot problems and tight calves since his teenage years or earlier, long before he began to run. Those problems came to a head six years
ago. He made a courageous decision to fix them once and for all with
surgery (photo above + more below).
Unfortunately, he's again suffering from a painful
foot condition at least partly caused by calves that are still much too tight.
THE FRUSTRATION OF PLANTAR FACIITIS
Last July Jim began noticing that one of his heels occasionally hurt after he ran. He
pretty much ignored it. Not good, in retrospect. Turns out, it was the
beginning of a nasty case of plantar faciitis (PF).
Most cases of PF are nasty. They develop slowly, sneaking up on you.
Once the symptoms are obvious enough to diagnose, they take what seems like forever to heal.

Jim at the Grand Teton 50-miler in early September
Why? Mostly because it's so doggone hard for runners to stop running
long enough for the fascia to heal properly. When it starts to feel a little better, they start running again. Then it gets further inflamed and hurts like the
dickens, especially when first putting foot to floor after getting out of bed
(hard floor is worse than carpeting). The runner stops running a few more days
and the foot begins to feel better. The runner again thinks it's healed
sufficiently to resume running . . .
Ad infinitum.
The cycle keeps repeating itself and the condition becomes
more chronic and more painful because the fascia doesn't get a chance to fully heal. It's just getting worse and worse, not better. We've heard of runners
suffering from PF for up to two years before it finally heals -- or they get
surgery.
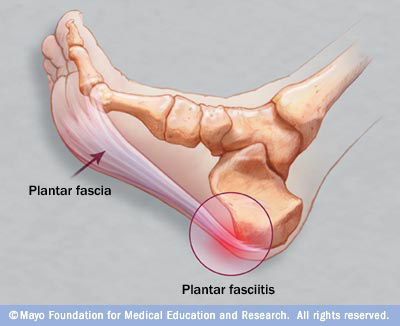
You can read all about the symptoms, causes, and treatments for PF at
the
Mayo Clinic and other reliable websites. This is a good graphic of the condition from the Mayo site:
Jim's in the fifth month of this insidious cycle. He didn't feel the pain
very often during July and August. He ran at least fifty miles comfortably at both the
Grand Teton and Hinson Lake races in September and his foot felt pretty good
after both events. By the last week of September, however, his foot began haunting
him. Maybe taunting is a better word.
That's when Jim finally told me about it. As soon as he described the
tenderness (no, pain!) in his heel when he first gets up in the morning, I knew
exactly what was wrong. "Dr. Norwood" diagnosed plantar faciitis before he
went to see our
chiropractor or an orthopedic PA.
How did I know? I've had PF previously, and the symptoms are just so
classic. Besides, it's one of the most common threads on the ultra list, coming
up regularly as yet another runner succumbs to the vicious cycle. I've got the
treatments memorized pretty well, in case I ever get it again.
WHAT CAUSED JIM'S PF?
The Mayo Clinic website lists several causes for the problem. Although it's
a common running injury, many non-runners get PF, too (even to the extent of
requiring surgery).
These are some
of the things that could have caused Jim's PF:
- Running long distances, especially over hilly terrain. It's what we
do!! He did a lot of running in the Rocky Mountains from May in the
Jemez to September in the Tetons. Even though he's used to lots of miles and
mountains, he may have over-done it.
- Older people tend to get PF more than younger people. Much as we hate to
admit it, we are "older" now.
- Jim's calves are extremely tight and have been at least since he
was a young Army recruit, years before he began running. Six years ago, when
he had bunions and Morton's neuromas removed on both feet at the same time,
he also had
gastroc recessions in both calves -- tendon
releases between the gastrocnemius and soleus to increase the range of motion
in his ankles and reduce the impact on his forefeet. (See photos below.) He still has
tight calves, and that can aggravate the Achilles tendon and plantar fascia.
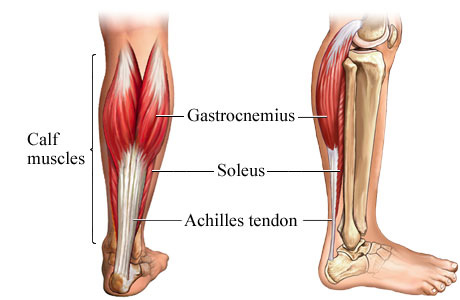
Graphic from this
website

Eight days post-surgery: stitches in one of Jim's calves
from the gastroc release

Frankenstein Feet! (eight days post-surgery when the
first bandages came off)

Jim's handsome new feet after they healed -- no more bunions or neuromas
- Even though Jim has worn orthotics prescribed by podiatrists,
orthopedists, or chiropractors for many years, he may still have some faulty
foot mechanics. Both high arches and flat feet can cause PF. Jim has high
arches.
- He may have switched too quickly from heavier trail shoes to lighter road
shoes during the summer, not allowing adequate time to get used to thinner soles, reduced
cushioning, and less arch support (even with orthotics).
I want to expand on the last possible cause.
A very popular running book called
Born to Run
came out in May or June. We ordered a copy after hearing rave reviews about it
on the ultra list. It was a good read, although I think that the personalities
of several of the runners who we know were exaggerated with some literary
license. Jim never did finish the book, but he got the gist of what it said
about learning to run more naturally.
The book has significantly popularized the "minimal shoe" and "barefoot
running" movements in the world of running, including trail ultra running. It
sounds great to switch to much less structured shoes for trail (even road)
running -- or going totally barefooted -- so you theoretically
run more naturally and have fewer injuries. But after wearing heavier, more
structured shoes for so many years, lots of runners are finding out the hard
way that it takes a lot of time to comfortably morph from your average trail or road shoe to the
minimalist models, or from minimalist shoes to barefoot running. Any big switch must be
done very gradually or most runners are asking for trouble.

Wolf Creek Greenway in Roanoke during
November (remainder of photos below)
Jim may have become one of the victims of this fad when he switched from
running most of his mountainous miles in Montrail and Asics trail shoes to his
lighter, less structured Asics 2140 road shoes. We don't know if this
caused his PF problem, but it may well have exacerbated it.
I also started wearing my lighter road shoes more this year because I'm
doing less running, more walking, fewer hills, flatter surfaces, and less
gnarly terrain. It's been a gradual process over two years, however. I'm
doing what I can to avoid ending up in the same predicament as Jim. It's bad
enough that I've got bum knees; I don't need bum feet. too.
HOW DO YOU GET RID OF PLANTAR FACIITIS?
You treat it early and aggressively, even if it means no running for several
weeks or months. That's very hard for most runners, including Jim and me.
It's been a long time since Jim had a milder case of PF so he did research on the internet and confirmed the treatments I
recommended: rest (reduced or no running), ibuprofen (NSAIDs =
anti-inflammatory), rolling his foot over a bottle of ice and/or our
ridged wooden foot roller, gentle stretching, cross-friction massage,
and wearing my old PF boot (padded plastic night splint) to bed every
night so the foot would remain at an angle of slightly less than 90
degrees all night to gently stretch the fascia (our feet are usually at
greater than a 90-degree angle during the day, and the fascia remains
tighter).

Jim complied with the ice, occasional ibuprofen, stretching his very-tight
calf, and self-massage. He did not completely stop running for a couple more weeks
but he did reduce the number of miles he ran and started walking more. He did
most of his miles on the rather flat, dirt Wolf Creek Greenway instead of hilly
or mountainous trails. He sat in the
whirlpool at the Y several times a week and used The Stick to massage the
bottom of his foot. He tried to sleep with the night splint but finally gave it
up after a couple weeks of poor sleep; he was never comfortable with
that. (On the other hand, I attribute the splint to finally "curing" my
case of PF several years ago.)
Jim resumed chiropractic adjustments in October and got ultrasound
on his foot two
or three
times a week for several weeks. Brian generously loaned him a portable
ultrasound unit to take with us on our trip so Jim can continue using it on his
foot. Jim isn't sure how effective these treatments are but he's doing them
regularly. Brian also gave him a different kind of orthotic to try, an
OTC brand instead of the custom-fitted inserts he's been wearing
for a while.

Meanwhile, we got some good calf stretching advice from two of our friends
who are medical practitioners. These are good even if you don't have PF --
excellent for prevention of both plantar faciitis and Achilles tendonitis:
- My massage therapist/yoga teacher recommended Jim do the "forward fold" for
five minutes at a time, at least once daily, to gently "remodel" and stretch
the muscle fibers in his calves. To do this stretch, sit on the floor with your
legs/feet straight out in front of you. The heels of your feet should be
against a wall, with the toes up at a 90-degree angle like when you're standing. Slowly lean your upper body forward until you feel a good stretch in your
calves. Hold for a minimum of two minutes and work up to five minutes at a
time. Breathe normally the whole time.
- One of our ultra running friends, an MD, recommended another
stretch that Jim prefers. She wrote: "Plantar F can be
tough to conquer. My favorite stretch is to put the good foot completely on a
step and the ball of the sore foot on the edge of the step. Then drop the heel
of the sore foot as low as it will go and hold for 7 minutes at least 3 times a
day. This will hurt to do especially in the calf, but it does stretch things
out and worked when I had it." Jim's been doing that with both feet, one at
a time, but hasn't worked up to seven minutes yet.
In early November Jim went in to see a PA at Roanoke
Orthopedics (it would have taken a couple weeks to see an orthopedist). She
advised him to purchase an OTC heel cup for his shoes (to be worn on top
of the new orthotic Brian gave him), take
2400 mg of ibuprofen a day to combat the inflammation more aggressively,
and continue with all the other treatments he was doing.
By then, Jim had already stopped running completely. Within a few days,
he also stopped aerobic walking, too. He could cycle and do weight
machines comfortably.
He was able to do yard work, run fire department calls, and do other
activities without pain.
He wasn't debilitated -- but his foot still hurt when he first got up
in the morning.

About ten days later Jim saw our primary care physician for his annual
physical. Jim told him about the plantar fascia problem and his frustration
that it didn't seem to be healing, in spite of all the things he was doing. The
doctor gave Jim
a "systemic" cortisone injection in the hip (not in the fascia itself;
as with the Achilles tendon, corticosteroids can weaken the plantar fascia
and make it susceptible to rupturing).
If you add up all the things Jim's been doing, you get ten or more
treatments. He's done just about everything he can, short of surgery.
SOME LIGHT AT THE END OF THE TUNNEL
After several weeks of no running or aerobic walking, Jim recently resumed walking
at the greenway for one to two miles at a time, every other day. So far, his
foot hasn't gotten any worse. He plans to gradually add in some running soon
and will assess how his foot feels after every session. He's slowly seeing some improvements
but will stop running again, if necessary, for however long it takes. He
asserts that he is
determined to fix the problem without having surgery, even if it means giving
up running for good.
Jim's been understandably depressed because he's as addicted to running
as I am. It's tough to give it up, even temporarily. His mood has improved
since he's begun walking more. It's those endorphins I keep telling you about!

Jim's not losing
the battle against PF quite as much any more, but it's too soon to
declare victory. He's still considering running/walking as much as he can at
the Run to the Future 24-Hour race in Phoenix at the end of December. If he
starts the race and can stay on the course only a few miles or hours, he'll
probably
join me as a volunteer for the remainder of the event.
There are at least three lessons here:
- do whatever is necessary to avoid getting plantar faciitis in the first
place
-
if you want to go minimalist or barefoot, do it very gradually
- if you get PF, treat it aggressively from the start
Next entry: hello from the Southwest!
Happy trails,
Sue
"Runtrails & Company" - Sue Norwood, Jim O'Neil,
and Cody the Ultra Lab
Previous
Next
© 2009 Sue Norwood and Jim O'Neil